Overview
Anterior cervical discectomy and disc replacement ore performed to relieve pressure on the nerves due to a prolapsed intervertebral disc or bone spurs, which are causing brachalgia (arm pain).
This operation is similar to an anterior cervical discectomy and fusion but a mobile artificial disc is placed in the disc instead of fusing the vertebrae together. There is evidence that the preservation of motion will protect the adjacent disc levels from developing excess stress and degenerative changes. As yet this is unproven, however it is known that the chance of requiring surgery next to a fused disc level is about 3% per year.
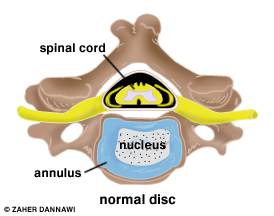
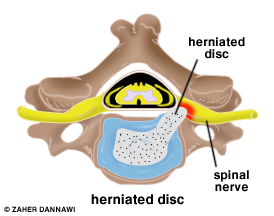
Figure 1. (Top view of vertebra). Degenerative disc disease causes the discs (blue and white dotted) to dry out. A tear in the disc annulus allows the gel-filled nucleus to escape and compress the nerve in its exiting canal (foraminal stenosis). The nerve becomes swollen and painful.
What is a cervical disc replacement?
The damaged disc will be reached from the front (anterior) of the spine through the neck area. By moving aside the neck muscles, trachea, and esophagus, the disc and bony vertebrae are exposed. Surgery from the front of the neck is more accessible than from the back (posterior) because the disc can be reached without disturbing the spinal cord, spinal nerves, and the strong neck muscles. Depending on your particular symptoms, one disc (single-level) or more (multi-level) may be removed.
After the disc is removed, the space between the bony vertebrae is empty. To prevent the vertebrae from collapsing and rubbing together, and to ensure motion preservation, a disc replacement is inserted.
Motion-preserving artificial disc replacements have emerged as an alternative to fusion. Similar to knee replacement, the artificial disc is inserted into the damaged joint space and preserves motion, whereas fusion eliminates motion. Outcomes for artificial disc compared to ACDF are similar, but long-term results of motion preservation and adjacent level disease are not yet proven.
Who is a candidate?
You may be a candidate for discectomy if you have:
diagnostic tests (MRI, CT, myelogram) show that you have a herniated or degenerative discsignificant weakness in your hand or arm pain worse than neck pain symptoms that have not improved with physical therapy or medication
A disc replacement may be helpful in treating the following conditions:
Bulging and herniated disc: The gel-like material within the disc can bulge or rupture through a weak area in the surrounding wall (annulus). Irritation and swelling occurs when this material squeezes out and painfully presses on a nerve.
Degenerative disc disease: As discs naturally wear out, bone spurs form and the facet joints become inflamed. The discs dry out and shrink, losing their flexibility and cushioning properties. The disc spaces get smaller. These changes lead to canal stenosis or disc herniation (Fig. 1).
The surgical decision
Most herniated discs heal after a few months of nonsurgical treatment. Approximately 10-20% of people with herniated disc problems have enough pain after 6 weeks of conservative treatment to consider surgery.
What happens before surgery?
You will be seen in the preassessment clinic, several days before surgery, where preoperative investigations (e.g., blood test, electrocardiogram) will be carried out. Some medications need to be continued or stopped before the day of surgery.
Stop taking blood thinning medications ( Warfarin and Clopidogrel) 7 days before surgery. Aspirin should also be discontinued 5 days before surgery. You should stop eating or drinking 6 hours before surgery; however, you can continue to have clear fluid (e.g water) up to 2 hours before surgery.
Smoking
The most important thing you can do to ensure the success of your spinal surgery is quit smoking. Smoking also decreases your blood circulation, resulting in slower wound healing and an increased risk of infection.
What happens during surgery?
You will lie on your back on the operative table and be given anesthesia. Once asleep, your neck area is cleansed and prepped.
An approximately 2-inch skin incision is made on the left side of your neck. The spine will be accessed by moving aside muscles in your neck and retracting the trachea, esophagus, and arteries. Finally, the muscles that support the front of the spine are lifted and held aside to see the bony vertebrae and discs.
With the aid of a fluoroscope (a special X-ray), a thin needle is passed into the disc to locate the affected disc. The vertebrae bones above and below the damaged disc are spread apart with a special retractor.
The outer wall of the disc is cut (Fig 2). Approximately 2/3 of your disc will be removed using small grasping tools, and then a surgical microscope will be used to remove the rest of the disc. The ligament that runs behind the vertebrae is removed to reach the spinal canal. Any disc material and bony overgrowths pressing on the spinal nerves and cord are removed to ensure an adequate decompression.
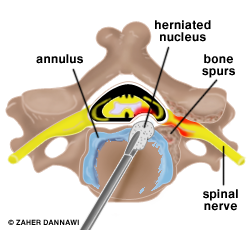
Fig 2. Disc removal
A disc replacement is then inserted in order to preserve motion and decrease the risk of developing adjacent disc disease (Fig 3).

Fig 3. C5-C6 & C6-C7 Cervical Disc replacement
What happens after surgery?
You will wake up in the recovery room. Your vital signs will be monitored. Any pain will be addressed.
You will increase your activity level (sitting in a chair, walking) either on the evening of the surgery or the next day. The drain will be removed on the 1st postoperative day. Most patients having a 1 or 2 level disc replacement are sent home the next postoperative day. However, if there are any concerns, you may have to stay in the hospital a bit longer.
Discharge instructions
Discomfort
After surgery, pain is managed with narcotic medication for a limited period (1-2 weeks).
Hoarseness, sore throat, or difficulty swallowing may occur in some patients and should not be cause for alarm. These symptoms usually resolve in 1 to 4 weeks.
Restrictions
Avoid bending your head forward or backward.
Do not drive for 2 to 4 weeks after surgery as your car insurers require you to be in full control of your car at all times without being distracted by pain . You are also required to be able to look over your shoulders otherwise you are considered unsafe to drive. DVLA require you to make an emergency stop.
You should not fly for 2 weeks following surgery.
Activity
You may need help with daily activities (e.g., dressing, bathing), but most patients are able to care for themselves right away.
Gradually return to your normal activities. Walking is encouraged; start with a short distance and increase it gradually . A physical therapy programme may be recommended.
If applicable, know how to wear a cervical collar before leaving the hospital. Wear it when walking or riding in a car.
Bathing/Incision Care
You may shower 1 to 4 days after surgery. Keep the dressing on for 10 days after surgey and dab it dry if it gets wet.
When to Call Your Doctor
If your temperature exceeds 38 degrees, or if the incision begins to separate or show signs of infection, such as redness, swelling, pain, or drainage.
If your swallowing problems interfere with your ability to breathe or drink water.
What are the results?
Pain from the procedure is usually limited and improves markedly within two to three days. Nerve symptoms such as pain, pins and needles and weakness are often dramatically improved within hours of the surgery, but in some cases can take weeks or even months to recover. Numbness is the last symptom to improve, but sometimes it does not recover. X-rays are obtained following surgery to confirm proper positioning and functioning of the disc replacement device. Most patients are capable of returning to light work within a week or two of surgery and to full duty six weeks following the procedure.
