What is a fusion operation?
Fusion simply means joining two bones together in order to decrease the movement at a specific motion segment.
Lumbar spine fusions can be performed from the front of the spine, (anterior approach) or from the back of the spine, (posterior approach). On occasions they may need a combined approach from the front and the back.
Bone or bone substitutes are used to fuse the bones together. Within the spine the bone graft may be placed posteriorly, between adjacent transverse processes (Posterolateral Fusion), or anteriorly, between the vertebral bodies (Interbody fusion). Certain techniques allow both fusions to be performed, resulting in a circumferencial fusion or 360 degree fusion. The bone may be stabilised with instrumentation, while the bone graft knits together.
Do you need fusion operation?
Fusions are performed within the lumbar spine for a variety of reasons.
Back pain, may be caused by a degenerate lumbar disc. Under these circumstances, a lumbar fusion aims to prevent movement between the adjacent vertebrae and therefore reduces the pain.
Instability of the spine may result in a spondylolisthesis, movement of one vertebra relative to the adjacent vertebra, which may lead to back pain or pressure on the nerves, which may cause leg pain. The spondylolisthesis may be reduced and fused, or under certain circumstances, fused in its slipped position.
Lumbar decompression surgery is used to relieve pressure on the nerves within the spine. If the spine is unstable or the process of the decompression results in the spine becoming unstable, then the decompression may be combined with a spinal fusion.
What other treatment options are there?
Injections into the spine
These procedures are used when pain relief is required, yet surgery is not immediately indicated. Leg pain may be relieved by an epidural or a nerve root block and back pain may be improved with facet joint injections. (See spinal injections)
Non fusion surgery
The spine may be stabilised without fusing the spine. Techniques include pedicle screws insertion into adjacent vertebrae and then connected together by a non-rigid structure (dynamic stabilisation). This has the advantage of maintaining movement within the spine, but may not be suitable for every condition. Suitability for non-fusion surgery depends on the type of problem within the spine and the severity of the condition.
Disc Replacement Surgery
Cervical disc replacement is becoming a widely used technique for the relief of arm pain secondary to cervical nerve root compression, however disc replacements within the lumbar spine has had a much more varied outcome and is not a universally accepted technique for the relief of chronic lumbar back pain.
Types of lumbar Fusion
Posterior lumbar fusion
Bone is placed between the transverse processes (TP) of adjacent vertebrae. (There are two TPs, one on each side of the vertebra, which project outwards). The bone placed between the two adjacent vertebrae heals to produce a solid fusion between adjacent vertebral bodies within the spine.
Frequently the spine is stabilised with screws and rods while the bone heals (postero-lateral instrumented fusion) (Fig 1).

Fig 1a. Posterior instrumented fusion L3-L5

Fig 1b. Lateral view Posterior instrumented fusion
PLIF or Posterior Lumbar Interbody Fusion
This technique allows circumferencial fusion of the spine as well as allowing decompression of the nerve roots (relieving the pressure on the nerves within the spine).
Pedicle screws are inserted in the same manner as for an instrumented postero-lateral fusion. The lamina at the back of the spine is then removed and the intervertebral disc between the vertebral bodies is removed. The nerve roots are then temporarily retracted out of the way to allow cages packed with bone graft to be inserted between the vertebral bodies.
The pedicle screws are connected together with the rods and more bone graft is placed between the transverse processes of the vertebral bodies, to obtain a fusion.
TLIF or Transforaminal Lumbar Interbody Fusion
This technique allows circumferential fusion of the spine but avoids removal of the lamina of the spine. It also causes less disruption to the posterior muscles of the spine, as the surgery can be performed between the muscles, rather than displacing them off the spinous processes.
Pedicle screws are inserted in the same manner as for an instrumented postero-lateral fusion. The facets joint at the back of the spine is then removed and the intervertebral disc between the vertebral bodies is removed. A single nerve root is then temporarily retracted out of the way to allow a curved cage packed with bone graft to be inserted between the vertebral bodies (Figure 2).
The pedicle screws are connected together with the rods and more bone graft is placed between the transverse processes of the vertebral bodies, to obtain a fusion.
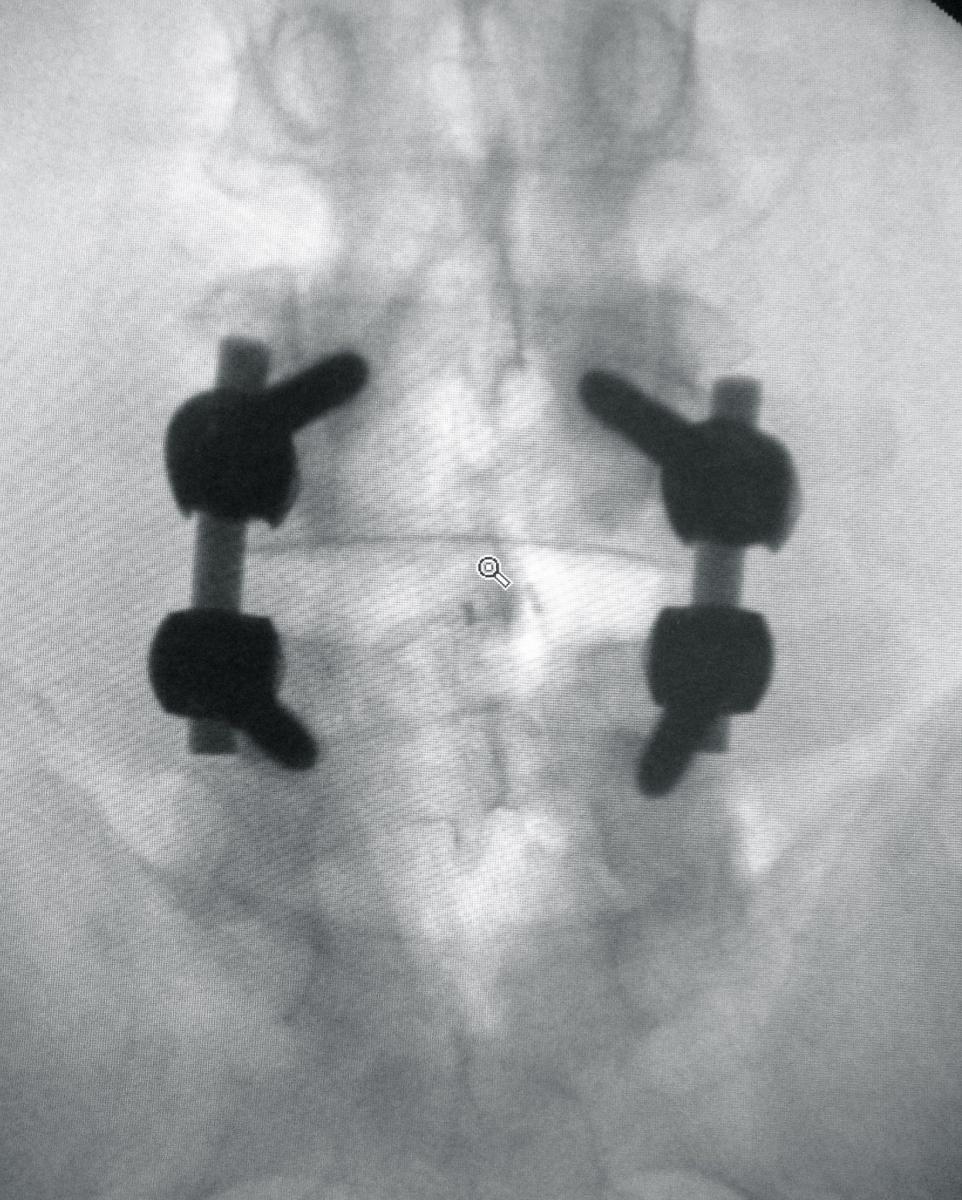
Fig 2a. AP view of TLIF at L4/L5
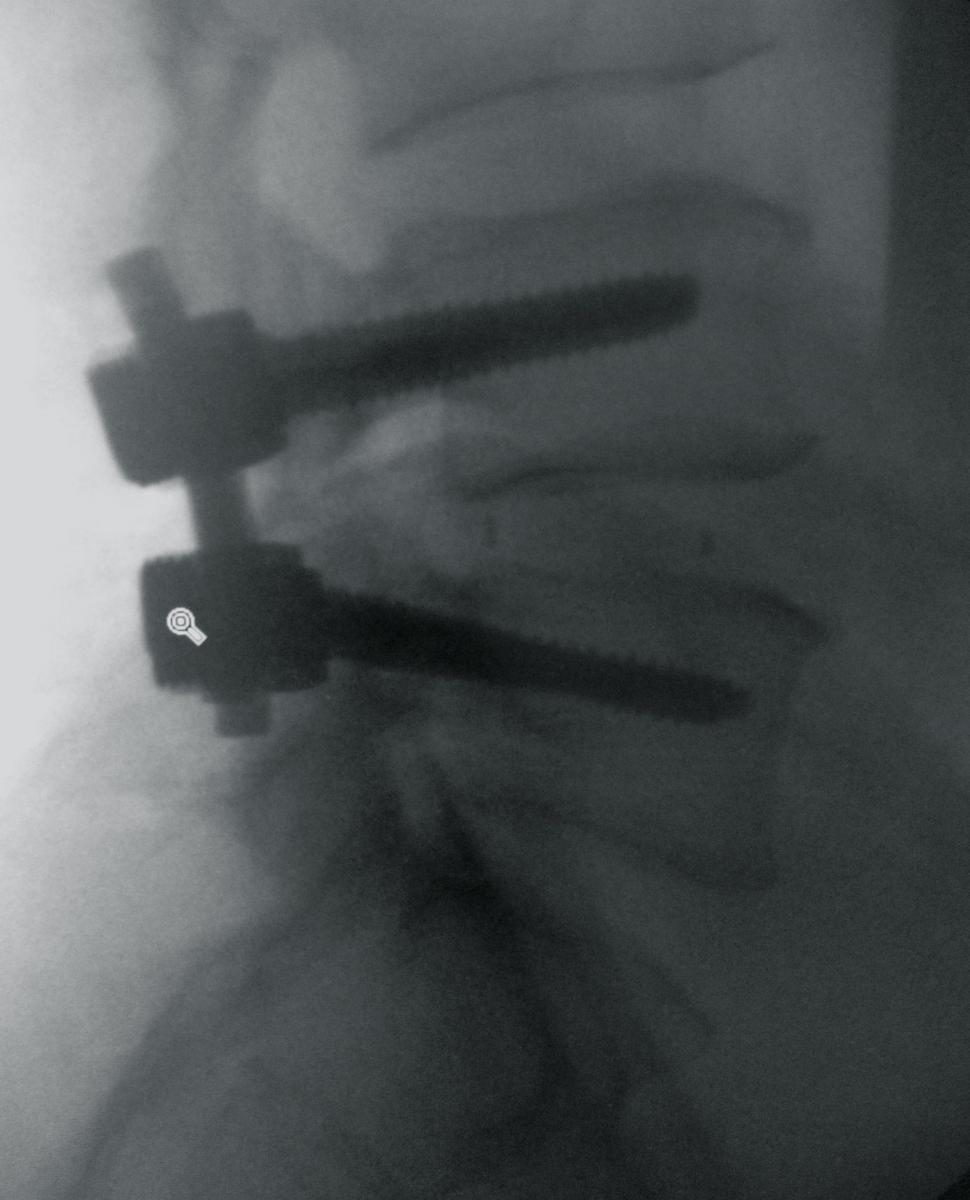
Fig 2b. Lateral view of TLIF at L4/L5
MIS interspinous fusion
The Aspen MIS Fusion System offers a minimally invasive implant option for spinal fusion. It has been shown to be comparable to screws in stabilizing the spine, which helps to address symptoms of back and leg pain at their source.
The Aspen device is a small, clip-like titanium implant that attaches to the spinous process, the bony parts of the spine located closest to the skin and away from delicate nerve roots ( Figure 3). Because of this, it can be implanted through a small incision while preserving surrounding muscle and tissue. The center of the Aspen device is also specifically designed to hold bone graft material that helps the body produce new bone to strengthen the spine.
Due to its minimally invasive nature, patients may experience a less painful and quicker recovery compared to patients with traditional pedicle screw fixation. Studies have shown the Aspen device provides robust stabilisation and promotes fusion while requiring a smaller incision, less muscle trauma, less blood loss and shorter surgery time.
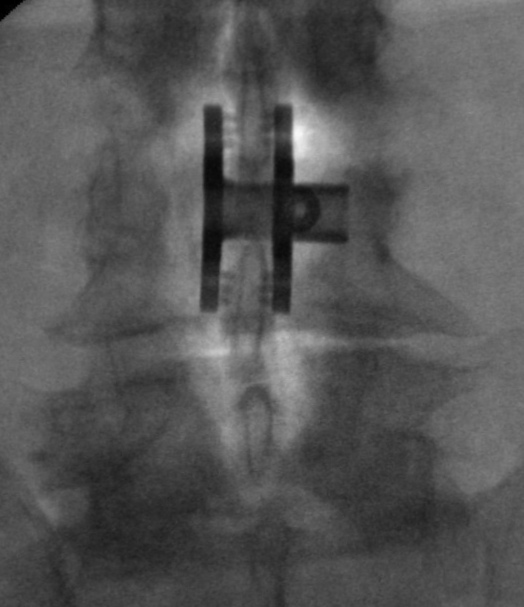
Fig 3a. AP view of the Aspen at L3/L4.
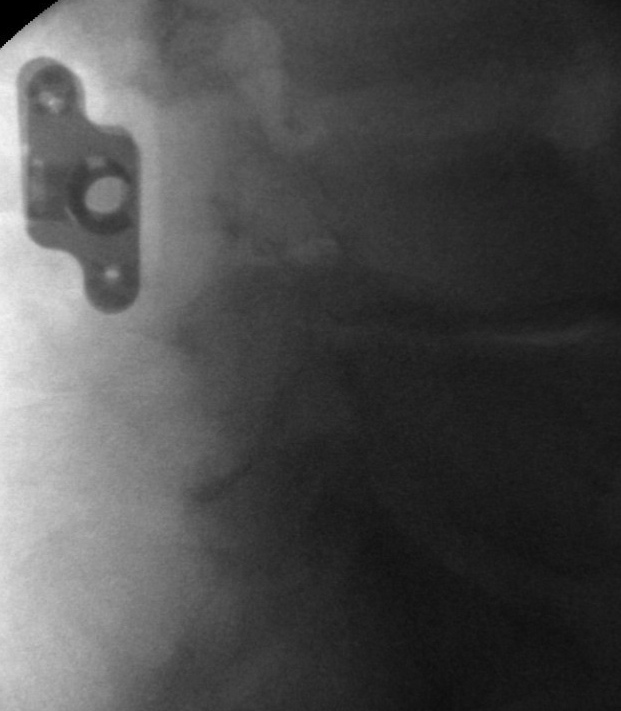
Fig 3b. Lateral view of the Aspen at L3/L4.
