Overview
Spinal stenosis is a frequently occurring and debilitating condition that limits patient’s activity levels.
Within the aging lumbar spine, thickening of the ligamentum flavum and increased size of the lumbar facet joints at the back of the spine cause narrowing of the canal (Fig 1)
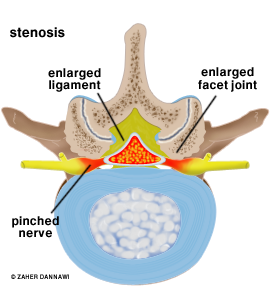
Fig 1: Spinal canal narrowing
This results in pressure on the nerve roots and central neural elements.
With exercise, patients may experience leg pain and describe a feeling of heaviness within the legs. The condition can be associated with lumbar back pain.
In an attempt to relieve the pressure on the nerves, patients tend to stoop forward when walking, rest intermittently and ultimately they are forced to limit their activity levels.
Natural History
The course of the problem has some uncertainty, but a general rule can by applied that with physiotherapy and analgesics 15% will improve with time, 70% will stay the same and 15% will deteriorate.
Prior to surgery
Prior to surgery you will be explained the natural history of the condition (what is likely to happen without treatment).
Other treatment options will then be discussed and the surgical procedure will be explained including the postoperative care and potential complications (see Complications), prior to you consenting to undergo the operation.
Spinal Decompression
A general anaesthetic is required and once this is administered the patient is placed on their front. An X-ray machine is used to localise the area of the spine that needs to be operated on.
The muscles around the spine are reflected out of the way, and then the soft tissues and bone, which is pressing on the nerves is removed. Sometimes the whole of the lamina at the back of the spine has to be removed to take all the pressure of the nerves (Fig 2), but in most cases a small window made in the lamina (a foraminotomy) allows adequate access to perform the decompression (Fig 3). The wound will be closed with absorbable stitches.
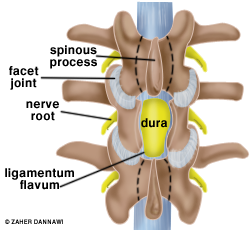
Fig 2: Decompression of the dural sac achieved by removing the lamina.
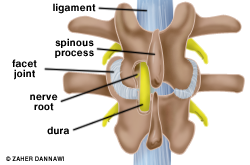
Fig 3: A window is made in the lamina (foraminotomy) to achieve a decompression.
Post operative care
On the evening of the surgery or the following day you will be able to mobilise with the help of the physiotherapist. You will be reviewed the day after surgery and the majority of patients will go home that day. You will be seen by a physiotherapist prior to discharge home and encouraged to mobilise as much as possible. Plans will be made for physiotherapy treatment within the outpatient department.
How long until I am better?
When pressure is taken off a nerve the first symptom to improve is pain, which may be immediate. It takes a longer time for muscle weakness to improve. If there has been any muscle wasting (loss of muscle bulk) this frequently never recovers, even though the strength often does. The last symptom to improve is numbness, which sometimes never recovers fully. After surgery it is not uncommon to have various aches and pains in and around the wound, and in the bony pelvis, hips and thighs. These usually improve with time. For the first few weeks postoperatively, your sciatica may return because of nerve swelling.
It is very helpful to see a physiotherapist before your surgery and even more important to see one postoperatively. You can receive heat, ultrasound and massage, information on exercises and on how to move and how to build up your core [back and abdominal] muscles long-term in order to help best maintain the strength of your back.
Patients usually return to work between four to six weeks following surgery depending on their job.
